Brief Description
This case is reported due to the rarity of suction dilation and curettage conversion to exploratory laparotomy. It is something providers should consent for, especially in the setting of suspected placental pathology.
Key Findings
-
Indications for dilation and curettage in this patient’s case included suspected cesarean scar pregnancy, noted on early ultrasound; a diagnosis of missed abortion; and the risk of hemorrhage without active management.
-
Indication for exploratory laparotomy was significant blood loss of approximately 1500 milliliters during dilation and curettage. Given prior and intraoperative ultrasound findings, providers in the case were concerned for morbidly adherent placenta with possible uterine invasion at the level of the cesarean scar. Bleeding was not resolved with more conservative measures, including attempted foley tamponade.
-
During exploratory laparotomy, providers were able to confirm that the uterus and adjacent structures were intact without damage. The patient’s hemorrhage was then able to be controlled through uterine artery embolization by interventional radiology.
Teaching Points
-
Cesarean scar pregnancy and placenta accreta spectrum are two conditions that may represent the same abnormalities of placental invasion at different times of gestation.
-
These pathologies carry profound risk of hemorrhage – even in the first trimester of pregnancy.
-
Additional research is needed to evaluate the best methods for bleeding prevention and management in patients with cesarean scar pregnancies and placenta accreta spectrum in early pregnancies. Ideally, such methods would allow for preservation of fertility if the patient so desired.
-
Providers performing dilation and curettage should remain cognizant of the risk for significant bleeding due to cesarean scar pregnancy and accreta spectrum pathology in any patient with risk factors for accreta.
-
Cesarean scar pregnancy and placenta accreta spectrum pathologies can be missed in early pregnancy losses and misdiagnosed as inevitable abortions due to lower uterine segment placement.
CASE
Background
Cesarean scar pregnancy (CSP) is an abnormal implantation in which the gestational sac embeds within the myometrium at the site of a prior cesarean section scar. Placenta accreta spectrum (PAS) describes a group of disorders characterized by abnormally adherent placental attachment, most commonly at the location of a previous uterine incision. CSP is typically diagnosed in the first trimester and is thought to represent an early form or precursor of PAS, which is more often identified later in pregnancy. Both CSP and PAS likely reflect the same underlying abnormal placental invasion occurring at different stages of gestation and are strongly associated with a maternal history of uterine surgery—including cesarean delivery, myomectomy, or dilation and curettage (D&C). Such procedures may create focal defects in the decidua basalis, exposing myometrium and permitting abnormal trophoblastic invasion. This process can result in deeply anchoring placental villi and progressive trophoblastic infiltration, significantly increasing the risk of severe hemorrhage and subsequent maternal morbidity and mortality.
The severity of PAS ranges from superficial invasion through the endometrium to full-thickness myometrial invasion and extension into adjacent pelvic structures such as the bladder, rectum, or peritoneum. Across the spectrum of CSP and PAS, hemorrhage remains the most critical and potentially life-threatening complication.
Much of the current research on disorders of placental attachment focuses on diagnosis and management of these conditions in the late second and third trimesters. While this is invaluable, there remains a guidance gap on how to approach abortive cases complicated by PAS and CSP in the first trimester. These early presentations, though rare, can similarly result in life-threatening hemorrhage that demands rapid, skilled intervention to mitigate.
Methods
This case report describes the history, presentation, and rapidly evolving clinical management of a first-trimester missed abortion in a pregnancy complicated by suspected cesarean scar pregnancy (CSP) versus placenta accreta spectrum (PAS). The case was initially diagnosed in early 2025. A subsequent chart review was conducted following the patient’s post-hospital clinic visit to monitor for complications during the month after discharge.
Results
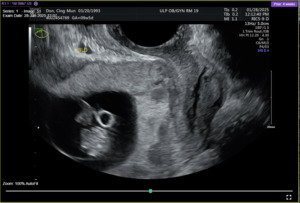
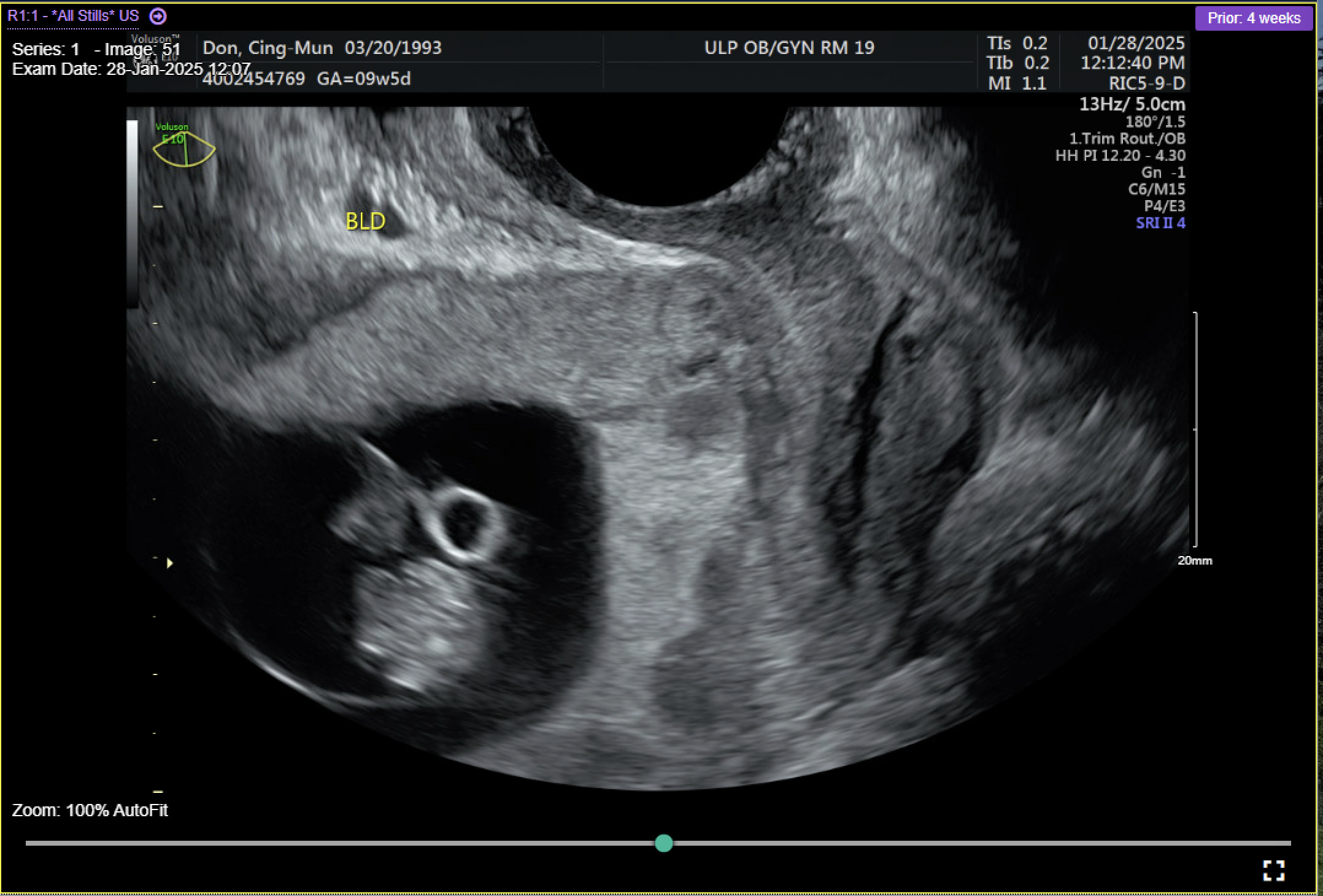
A 31-year-old gravida 2 para 1001 at 13 weeks and 6 days gestation by a 7-week ultrasound presented to ULH for surgical management of a missed abortion in the setting of suspected CSP versus PAS. The patient had previously been seen at an outside hospital emergency room for concerns of bleeding and pelvic pain. Ultrasound workups for these concerns were significant for viable intrauterine pregnancy and moderate subchorionic hemorrhage superiorly, grossly measuring 5 cm at the largest dimension. Two weeks after her initial emergency department (ED) visit, the patient was seen in our practice’s general obstetric clinic. A first trimester ultrasound was performed at this time and again demonstrated a 5 cm subchorionic hemorrhage (Figure 1). At this time, concern for CSP versus PAS was also noted, and the patient was advised to return for a follow-up scan. When the patient returned for further evaluation of placental pathology, ultrasound revealed fetal demise with absent fetal cardiac activity (Figure 2). Following discussion with the maternal fetal medicine (MFM) provider, the patient ultimately elected for surgical evacuation of the products of conception to mitigate spontaneous bleeding risks in the setting of CSP versus PAS.
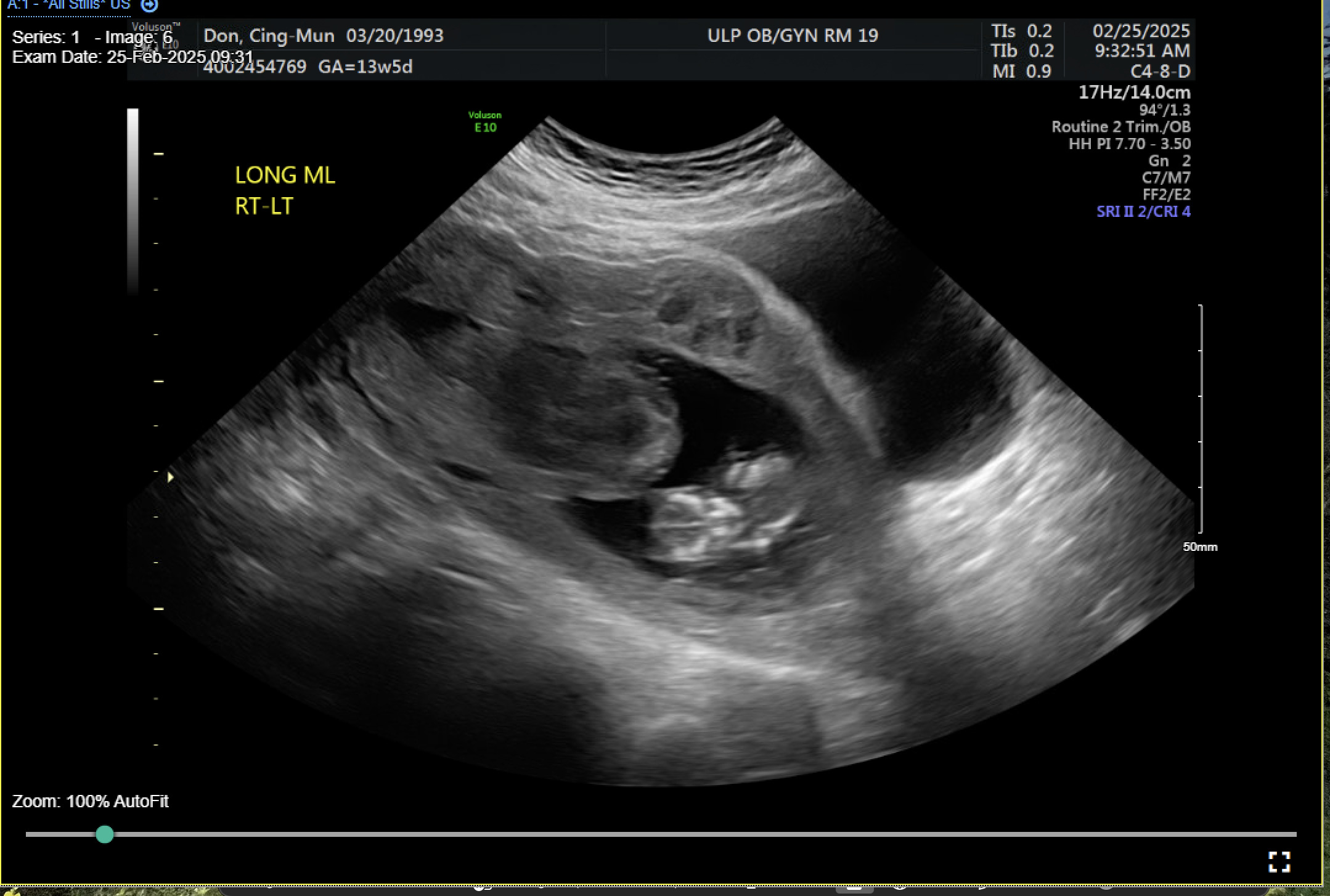
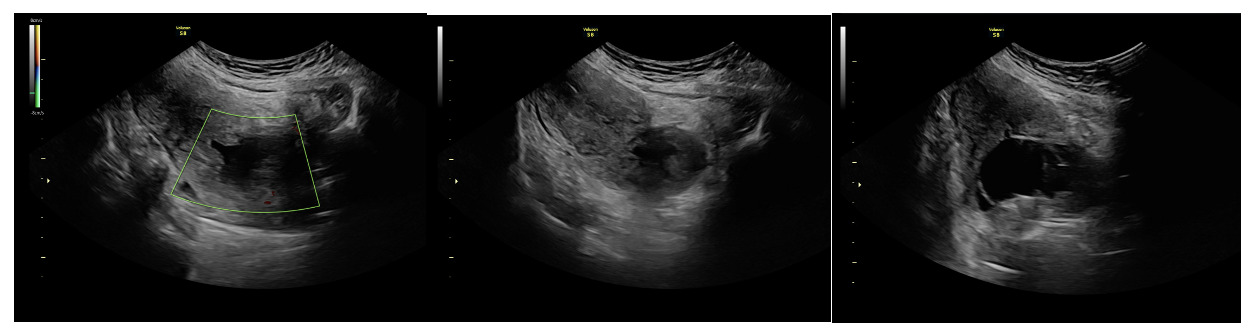
On admission for planned D&C, consents for laminaria placement, suction dilation and curettage under ultrasound guidance, possible uterine artery embolization, and possible hysterectomy were discussed and signed. The patient then underwent successful placement of a large and a medium-sized laminaria without complication. She subsequently underwent suction D&C with ultrasound guidance (Figure 3). Despite the prophylactic placement of 400 micrograms of rectal misoprostol and the administration of 20 units of Pitocin in IV fluids at the start of the case, the patient experienced significant hemorrhage during the procedure with an estimated blood loss of 1500 mL. Intraoperative findings raised concern for uterine rupture (Figure 4). A Foley balloon inflated with 30cc of saline was placed for attempted intrauterine tamponade (Figure 5), and a brisk blood loss of 500 mL immediately filled the foley catheter bag. Vaginal packing and intramuscular methergine were given as additional attempts to control the bleeding, but the patient’s hemodynamic status rapidly deteriorated. This necessitated volume resuscitation and transfusion of two units of packed red blood cells. An emergent exploratory laparotomy was then performed to identify the source of the bleeding with preparedness to repair any defects or perform a hysterectomy to prevent exsanguination. A thorough survey of the uterus, adnexa, and adjacent pelvic structures revealed no overt source of bleeding, uterine rupture, or organ invasion. The uterine and bladder serosa were intact. No hemoperitoneum was found. Further inspection revealed no additional blood loss beyond the 500 mL noted in the foley bag. Blood loss was ppropriately corrected for, and the patient became hemodynamically stable. The abdomen was closed, and the patient was transferred to interventional radiology for uterine artery embolization, prevented additional bloodloss. Following embolization, the patient was noted to be stable and extubated without issue.
On postoperative day 1, the intrauterine Foley catheter balloon was removed without recurrence of bleeding. The patient recovered well, resumed a regular diet, ambulated independently, and opted for Nexplanon insertion for contraception. By discharge on postoperative day 3, she reported only scant vaginal bleeding and remained hemodynamically stable. At an outpatient follow-up appointment two weeks after her hospitalization, the patient reported that she was recovering well. It was recommended that repeat imaging of the patient’s uterus occur within the next 6 months, and that the patient should schedule an MFM preconception consultation prior to any attempt at future pregnancy.
Discussion
This case highlights the rare but serious complication of significant hemorrhage during first trimester D&C in a patient with suspected CSP versus PAS pathology. Although placenta accreta is typically associated with second and third-trimester morbidity, its presence in early pregnancy as CSP poses an equally significant risk for life-threatening hemorrhage. Our patient’s course highlights several key considerations. First, pregnancies with overly adherent attachments - regardless of age of gestation - can present with significant hemorrhage that is unresponsive to routine uterotonics and tamponade techniques. Second, preoperative recognition of PAS, while critical, does not eliminate the potential for intraoperative instability, necessitating a multidisciplinary team that includes surgical, anesthetic, and interventional radiology support. Finally, this case illustrates that fertility-sparing hemorrhage management via uterine artery embolization is possible in select cases featuring rapid diagnosis and coordinated care.
Conclusion
Cesarean scar pregnancy (CSP) and placenta accreta spectrum (PAS) are forms of abnormally adherent placentation that have become increasingly prevalent alongside rising rates of uterine procedures, particularly cesarean delivery. Such procedures may disrupt the endometrial–myometrial interface, creating abnormal implantation sites for future pregnancies. Both CSP and PAS carry substantial risks of maternal morbidity and mortality due to hemorrhage — risks that are not confined to third-trimester deliveries, but may also arise during first-trimester gestations. A high index of suspicion, timely diagnosis, meticulous preoperative risk stratification, access to multidisciplinary care, and early planning for hemorrhage control are essential to optimizing maternal outcomes. Greater awareness and clearer management guidelines are also needed to support clinicians caring for patients with CSP and PAS, especially when these conditions present outside the typical gestational window.