1. Introduction
Contraception is an important topic of conversation among patients and their providers. Discussions often focus on both reversible and nonreversible forms of contraception, and there are various contraceptive options available to men and women, with each option utilized by various populations. While many options of birth control exist, female permanent contraception surgery is the most commonly used method for women aged 15-49, with over 18% of this population utilizing this method in 2015-2017 (“FastStats - Contraceptive Use” 2023).
There are different ways to perform a female permanent contraception surgical procedure also known as “tubal ligation”. The various ways are partial or complete salpingectomy, bipolar cautery, placement of occluding clips or rings and these techniques can be performed with either a mini-laparotomy incision or a laparoscopic procedure (Stuart and Ramesh 2018). Postpartum tubal ligation is typically performed using an infra-umbilical mini-laparotomy incision and is considered a safe surgical procedure. There are very few reports of major complications (Richardson, Hall, and Zuckerwise 2018). Postoperative complications have been reported to be as low as <0.5%, with the primary complication being patient regret (Richardson, Hall, and Zuckerwise 2018). Other morbidity events that have been studied include anesthetic complications, surgical site infections, bleeding, bowel or vascular injury, and risk of ectopic pregnancy. One study comparing rates of post operative morbidity in obese and non-obese patients showed composite morbidity rate to be approximately 1.3%, and it was comparable across all BMI categories (Byrne et al. 2020). However, the benefits to performing this procedure in the immediate postpartum period are largely due to ease of access and assurance that patients are not pregnant at the time of their surgery (Mercier et al. 2019).
Because this is a safe and permanent birth control method, many women desire this for their contraception. However, only about 50-60% of these patients have this procedure completed prior to hospital discharge (Mercier et al. 2019). There are multiple known barriers to completion of this procedure including age, Medicaid consent form status, and obesity, however, there are poor outcomes if this procedure is not completed during this immediate time period. Almost 70% of pregnancies after a delayed tubal ligation surgery are unintended, with over 45% of patients becoming pregnant in the first year (Byrne et al. 2020). It is also known that low income and minority women are at the greatest risk of unintended pregnancy, and Borerro et. al. calculated a cost effectiveness model to determine the economic burden of unfulfilled tubal ligation due to the Medicaid consent policy (Borrero et al. 2013). Their model estimated about 113 avoidable unintended pregnancies per 1000 women desiring a federally funded tubal ligation procedure, which could equate to a financial burden of $371 million (Richardson, Hall, and Zuckerwise 2018). Additionally, there are large financial burdens to the family, with the U.S Department of Agriculture estimating the average cost to raise a child in a middle-class family in 2015 to be $284,570 (Lino, n.d.).
These estimated financial burdens of unintended pregnancy are massive for both the healthcare system and the families. This emphasized the importance of providing contraception when patients desire and to make every attempt to avoid any delay in the surgical plan.
Logistical barriers play a large role in the completion of post-partum sterilization procedures. The most common system-based barriers include federal consent form status and lack of anesthesia or operating room (OR) availability. Some studies noted that attempting to schedule the procedure later in the week (Wednesday – Sunday) significantly impacted OR and anesthesia availability (Flink-Bochacki et al. 2019). Patient factors also impact unfulfilled postpartum completion of the procedure. Many reasons documented include patients changing their mind as well as a patient’s desire to avoid NPO status for a prolonged period of time.
Although there is clear data reporting 50-60% of patients not having their desired tubals completed prior to discharge, there is no definite data on what percentage of these patients have their sterilization procedure completed within the next 12 months. Because the financial burden is estimated to be high, having a clear data point can benefit future policies and guidelines regarding immediate postpartum tubal ligation. If interval tubal completion rates are as low as anticipated, this can provide evidence that policies may need adjustment. This data can potentially affect how likely surgeons are to perform surgery, how Medicaid consent policies should be adjusted, encourage providers to identify and problem-solve systemic and institutional barriers against timely surgical care.
The goal of this study is to determine the true completion rates of interval tubals within 12 months following delivery to further understand how barriers may have lasting effects and potentially lead to increased healthcare costs. We hypothesize that the completion rates will be low, emphasizing the importance of removing barriers and completing surgery immediately postpartum prior to hospital discharge.
This project seeks to add literature regarding postpartum tubal ligation completion rates in patients who desired permanent contraception procedures at the time of their delivery hospitalization. Approximately 50-60% of patients do not have their tubal ligations completed prior to discharge from the hospital, however there is no data reporting what percentage of these patients have their desired tubals completed within 12 months of their delivery. This study aims to answer that question and provide further information regarding barriers that exist for this sub-group of patients. The outcomes of this study can provide power for adjustments to future legislative, systemic, and institutional policies and guidelines regarding immediate postpartum tubal ligation.
The objectives of this study are the following: 1) Determine the percentage of women desiring an immediate postpartum sterilization procedure at the time of admission for delivery, 2) Determine the percentage of patients who do not receive their immediate postpartum tubal sterilization prior to discharge from delivery, 3) Determine the percentage of patients who then complete their tubal ligation procedure within 12 months of discharge from delivery, 4) Determine the reason for failure of postpartum tubal completion prior to discharge from the hospital, and 5) Potentially provide data for policy and guideline changes regarding patient qualification for immediate postpartum tubal ligation surgery.
2. Materials and Methods
This was a retrospective cohort study. Participants included individuals aged 18 years or older who gave birth at the University of Louisville Hospital (ULH) and desired a postpartum tubal sterilization during their hospitalization for delivery from January 1, 2019 to January 1, 2022. Exclusion criteria excludes individulas under the age of 18 and those who no longer desired postpartum tubal sterilization at the time of admission for delivery. As this is an exploratory study, no sample size was estimated, and we plan to use any available data that can be collected during the inclusion dates noted above.
Both primary and secondary outcomes will be analyzed. Primary outcome includes percentage of patients who complete their sterilization procedure within 12 months of discharge from the hospital. Secondary outcomes include the percentage of patients who desired immediate postpartum tubal sterilization and did not have this completed prior to discharge from delivery, the percentage of patients who did not receive an interval tubal sterilization procedure within 12 months of delivery and became pregnant, and the reason for failure of postpartum tubal completion prior to discharge from the hospital.
Data collection for this experiment will be conducted via a retrospective medical chart review of the participants’ electronic medical records. Eligible patients will be selected through manual review of the electronic medical record system using ICD-9 and ICD-10 codes. Only data that pertains to the study will be extracted and entered into a secure REDCap database. All protected health information will be securely entered into this REDCap database.
Identification of eligible participants will be based on women aged 18 years or older who were delivered at UofL Hospital who desired a postpartum tubal sterilization during their hospitalization for delivery from January 1, 2019 to January 1, 2022. All eligible participants in this time period will be included in the study. Data collection for this experiment will be conducted via a retrospective medical chart review of the participants’ electronic medical records. Eligible patients will be selected through manual review of the electronic medical record system using ICD-9 and ICD-10 codes. As this is a retrospective cohort study, participants will not be contacted for participation in this study.
3. Results
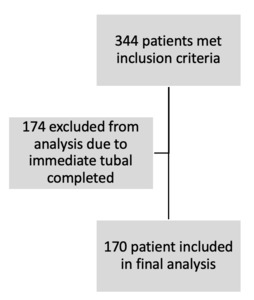
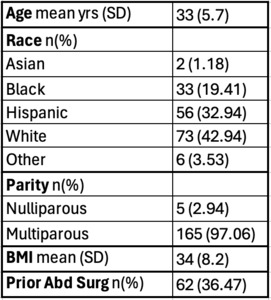
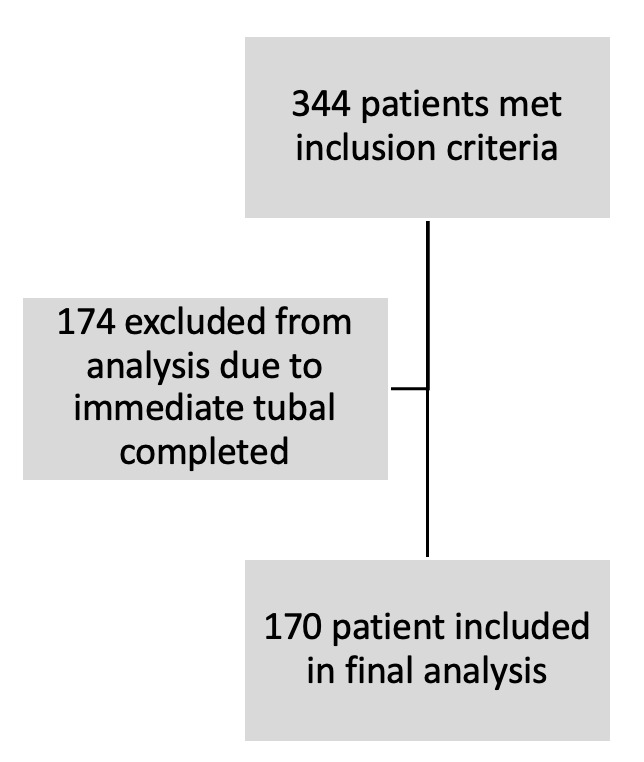
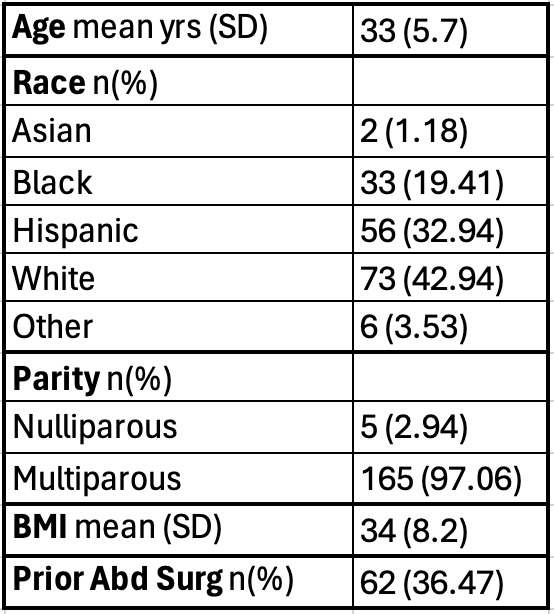
344 patients were identified and met inclusion criteria for the study. Of those 344 patients, 174 patients had an immediate postpartum tubal sterilization completed at the time of admission for delivery. This left 170 patients who were included in the final analysis regarding interval tubal sterilization, as seen in Figure 1. Table 1 outlines the demographic information of these patients. The average age of the patients who did not receive an immediate postpartum tubal sterilization was 33, and 1% identified as Asian, 19% identified as Black, 33% identified as Hispanic, 43% identified as White, and 4% identified as Other. 3% of these patients were nulliparous, and the remaining 97% were multiparous. Their average BMI was 34, and 36% of these patients had a history of some prior abdominal surgery.
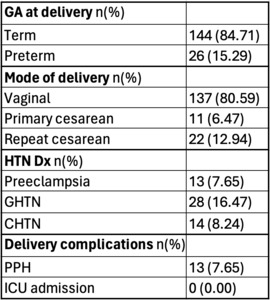
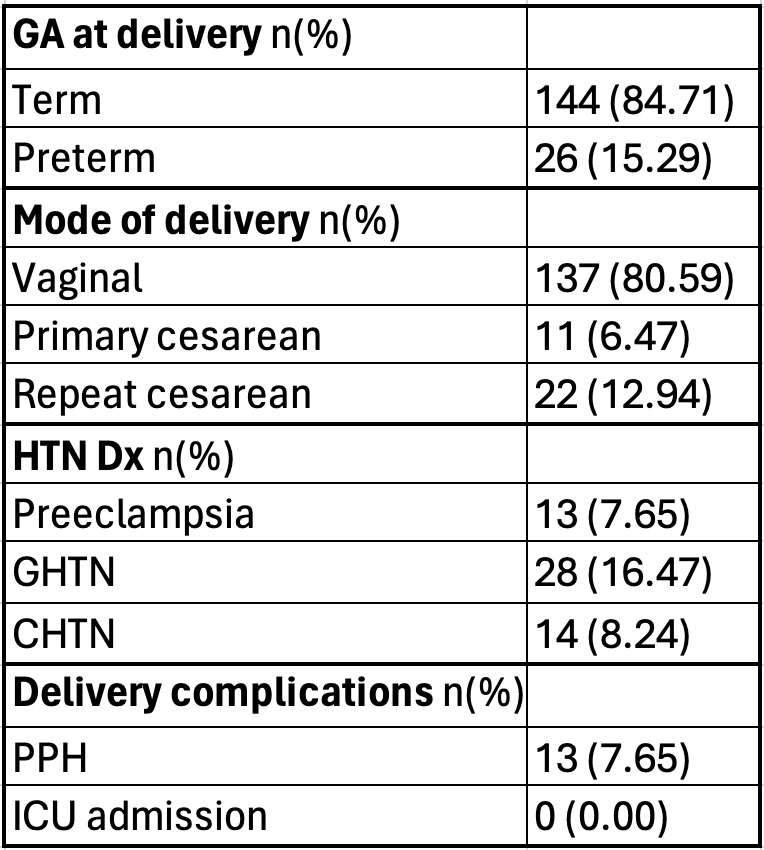
Table 2 identifies maternal outcomes at the time of delivery. 85% of patients who desired an immediate tubal but did not have this completed had a term delivery, and 15% had a preterm delivery. 81% of the deliveries were vaginal deliveries, 6% were primary cesarean section, and 13% were repeat cesarean sections. Both primary and repeat cesarean sections were not scheduled but were recommended at some point during the labor induction process. A total of 32% of patients had a diagnosis of hypertensive disorders of pregnancy, with the breakdown listed in Table 2. 8% of these patients had a postpartum hemorrhage at the time of delivery, and no patients were admitted to the ICU.
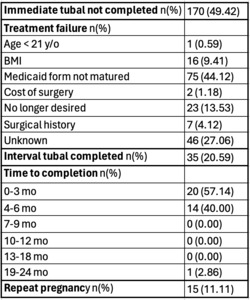
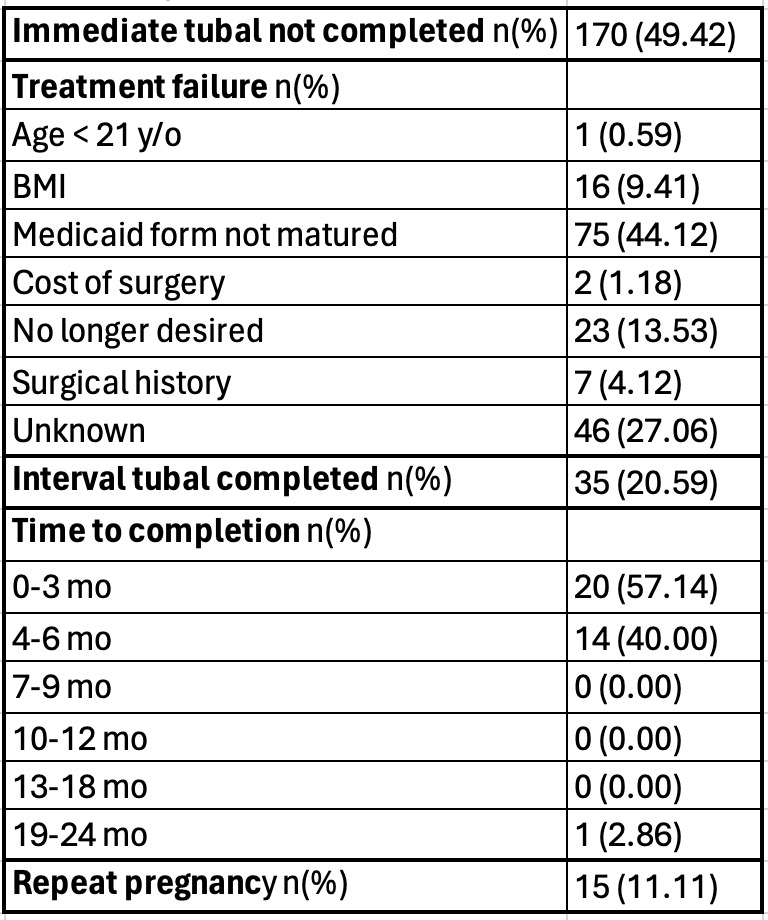
Table 3 identified tubal outcomes in the group of patients who did not receive an immediate tubal sterilization at the time of admission for delivery. 49% of patients did not receive their immediate desired tubal. Treatment failure is defined as patients who desired the immediate tubal but did not receive this in the immediate postpartum course. The most common reasons for treatment failure were listed as age < 21 years-old (1%), BMI (9%), Medicaid consent form not matured (44%), cost of surgery (1%), patient no longer desired a tubal in the postpartum period (14%), patient’s surgical history (4%), or unknown cause (27%). Of these patients who did not have their immediate tubal completed, only 21% had an interval tubal completed. 97% of patients had this completed within 6 months of delivery, and 3% had this completed within 19-24 months from delivery. 11% of patients were then pregnant again within 24 months.
4. Discussion
Our hypothesis was that there would be a low completion rate of interval tubal sterilization. This study confirmed the hypothesis, as only 21% of patients had their interval tubal completed. This data adds to the paucity of data existing regarding interval tubal completion rates and emphasizes the importance of immediate postpartum tubal completion. It also provides data regarding rising costs for families and the healthcare system and helped identify our hospital’s most common barriers to immediate tubal completion. Our immediate completion rate of 50% is consistent with most studies; however, identifying hospital specific barriers can allow for improving access to patient’s desired contraception. Of the 21% of patients who had their interval tubal completed, 97% of them had it completed in 6 months. This emphasizes the importance of close follow-up, continuity of care, and surgical scheduling.
There were many strengths of this study including a large sample size as well as all charts being reviewed manually by one provider and thus limiting selection bias. However, because this was a retrospective study, that does introduce more risk for bias. Other limitations of this study include the data point ending in 2024, so it is possible additional patients may still have had interval tubals completed that were not accounted for. There was also some incomplete documentation, with some charts not listing a reason for not completing an immediate postpartum tubal. This made the analysis challenging, as these unclear charts were then labeled as “unknown.” In addition, patients may have had their interval tubal completed at a different hospital system, which could falsely lower our interval completion rates. Possible future directions include focusing on why patients do not have interval tubal sterilization completed after 6 months. This could be related to insurance coverage, difficult reestablishing care, versus other barriers that need to be addressed. Because the lack of maturation of the Medicaid consent form was the most common barrier to care in our hospital, it may be advantageous to find a way to standardize the gestational age that we review this form with our patients. This could allow more patients to receive their desired form of contraception at the time of admission for delivery.
In conclusion, 51% of patients who desire an immediate postpartum tubal ligation at our hospital have this completed prior to discharge. Of the 49% who did not have an immediate surgery, only 21% had their interval tubal completed. 97% of patients who had their interval tubals completed, had this done within 6 months of delivery.