1. Introduction
By 2100, the US Centers for Disease Control and Protection and other sources estimate that ~200–400 million people will be born thanks to Assisted Reproductive Technology (ART)/In Vitro Fertilization (IVF) (Faddy, Gosden, and Gosden 2018). The increasing demand for ART/IVF services, including cryostorage, compounded by a growing number of unclaimed reproductive specimens and updated laws that permit longer cryostorage will lead to a heavier workload, on-site cryostorage shortages, and related challenges, issues, and risks (Alikani 2018; Alikani and Parmegiani 2018; Alikani et al. 2014; Campbell et al. 2022; Canosa et al. 2023; Go 2019; Niederberger et al. 2018; Rienzi and Fauser 2021; Rinehart 2021; Simione and Sharp 2017; Simon 2021; Simopoulou et al. 2019; Tomlinson 2018; Priddle et al. 2022). In turn, these challenges will create stressful working conditions for ART/IVF providers, opening the room for error and potential for mishandling of reproductive specimens, especially since many IVF clinics still rely on handwritten labels, paper ledgers/Excel spreadsheets, and manual monitoring of cryostorage conditions (Castilla et al., 2014; Alikani 2018; Schiewe et al. 2019; Go 2019; Murphy et al. 2022; Palmer et al. 2022; Murphy et al. 2023; Murphy et al., 2024). In recent years, some of the reported errors have led to devastating consequences for the patient(s) and legal implications for the providers, as per published literature and news reports (Letterie 2017; Letterie and Fox 2020; Moutos, Lahham, and Phelps 2019; Rasouli, Moutous, and Phelps 2020; Murphy et al., 2022b; Applebaum et al. 2023; Klipstein and Daar 2023).
In 2020, Letterie and Fox identified 133 lawsuits filed in state and federal courts in the U.S. over a 10-year period (January 1, 2009, to April 22, 2019; Letterie and Fox 2020). During this period, US-licensed ART/IVF clinics performed 398,256 embryo-thaw procedures. On the basis of their legal findings and the ART/IVF clinics statistics, the authors estimated the IVF incidents to be infrequent (<1%). However, there is no direct way of estimating the frequency of IVF incidents in the U.S., since CDC and SART only mandate U.S. ART/IVF clinics to report success rates (Centers for Disease Control and Prevention 2024; Society for Assisted Reproduction Technology, n.d.), and most legal cases are handled before reaching court or settled out of it, protecting the information from the public by non-disclosure agreements (Bernstein and Torbati 2024).
To our best knowledge, only UK Human Fertilisation and Embryology Authority (HFEA) requires licensed ART/IVF clinics to report IVF incidents on an annual basis, and this data is included in the annual State of the fertility sector reports. There were no Grade A (most severe) incidents in the latest reporting period (HFEA 2022/2023), and the number of Grade B (severe; 225/517, 44%) and Grade C (291/517, 56%) incidents remained consistent with previous years (2022/23 report). However, the mandatory reporting does not guarantee that all incidents have been captured and mitigated. Some incidents go unnoticed for months, years, and even decades, as shown in the cases of accidental sperm mix-ups (BBC 2016; Campoamor 2021) or deliberate fraud by providers (Cecco 2021; Horton 2020; Vanderveen 2018). The latter category was excluded from our analysis since we only focused on unintentional IVF incidents.
Since IVF incidents and resulting legal cases vary in severity, scope, and outcomes, and local legal and regulatory environment for patients and ART/IVF providers, the present study seeks to identify the causes of lawsuits against ART/IVF providers, and how the legal outcomes varied between cases and countries, and the emotional and reputational damage to patients, their families and providers.
2. Materials and Methods
2.1. Literature Review
A review of legal cases was conducted using Lexis Nexis, Westlaw, Bloomberg Law, and CaseLaw databases, newspaper and magazine articles, legal reviews, peer-reviewed journals, and online publications. The key terms for the search included IVF incidents, IVF lawsuits, embryo mix-ups, sperm mix-ups, embryo/sperm/egg damage and loss, storage failure, tank failure, and others. Data published by the Centers for Disease Control, Society for Assisted Reproductive Technology (SART), and HFEA contributed to the review.
Public data regarding the count, type, and geographical location of IVF incidents, resulting legal cases, and legal, reputational, and monetary outcomes for patients and providers were collected from without restricting it to a set period of time, and with the last search performed on April 30, 2023. Legal cases were categorized based on the nature of the reproductive specimen (egg, embryo, and sperm) and the type of incident (damage, loss, mishandling, mix-up, etc.). The U.S. and international cases were analyzed separately and together. To analyze the data, we performed a basic descriptive analysis using Microsoft Excel. To avoid skewing, storage-related incidents involving large-scale incubator, freezer, and liquid nitrogen tank failures were analyzed separately due to the number of affected patients per incident being in the hundreds and reproductive specimens in thousands.
2.2. Study objectives
The objectives for this study were to determine (1) the number of mixed-up, ruined IVF experiences that translate into the number of families/births missed or hurt due to IVF accidents and human error; (2) the number of patients affected, including single parents and couples; (3) the amount of pay-out from the above mix-ups and/or the financial impact of these incidents on clinics, individual providers, and patient families; (4) the number of specimens impacted; (5) the stress created and/or family crisis imposed because of these incidents; and (6) the technical details of IVF failures that led to embryo loss, damage, or misplacement, and how it came to light/what source it was reported in.
3. Results
3.1. Global legal cases by country
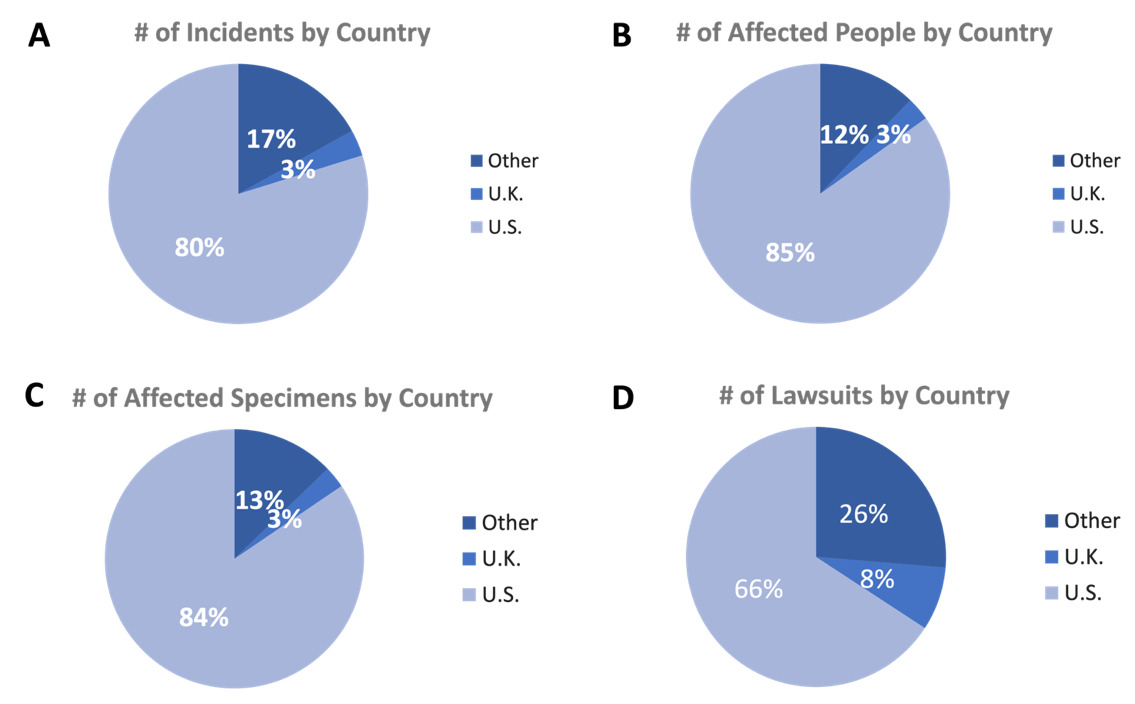
As of April 1, 2023, we identified 215 legal cases worldwide, which affected 2183 people and 8453 specimens, resulting in 259 initial lawsuits (Table S1; for the U.S. breakdown, see Tables S2 and S3; for the breakdown for the rest of the world, see Tables S4 and S5). After excluding 10 cases of catastrophic large-scale storage, tank, and alarm failures and power loss to avoid data skewing, 205 cases were attributed to specimen mix-up, damage, mishandling, loss, and possible contamination (84.9% cases in the U.S., 2.9% in the U.K., and 12.2% in other countries). These cases affected 307 people (79.8%, 3.3%, 16.9%) and 258 specimens (84.5%, 2.7%, 12.8%), resulting in 76 initial lawsuits (65.8%, 7.89%, 26.3%) (Figure 1). Specimen mix-ups were the most prevalent type (88.2%).
3.2. Large-scale storage, tank, and alarm failures worldwide
The 10 failed storage, tank, and alarm incidents caused the most damage, affecting more than 1800 patients and more than 8,100 specimens and resulting in 181 initial lawsuits (Table 1). Owing to the size and scope of the incidents, most of these cases were consolidated into class action suits.
In the landmark case of the 2018 tank failure at the Pacific Fertility Center in San Francisco, California, USA, which destroyed ~3500 frozen eggs and embryos for 400 patients, a federal jury awarded $15 million to five families, which were included in one of several class action lawsuits against the clinic (Hawkins 2021). Ninety percent of the award was assigned to the tank manufacturer and 10% to the clinic. This case was, however, appealed by the tank manufacturer and settled out of court, with the final award amount protected by a nondisclosure agreement (Bernstein 2023).
In another case, also in 2018 of a loss of ~4000 frozen eggs and embryos of 950 patients took place at University Hospitals Cleveland Medical Center in Cleveland, Ohio, USA. The loss occurred because of a turned-off remote alarm system on a storage tank. Initially, the fertility laboratory lost its accreditation. The accreditation was regained after implementation of system changes to protocols and the laboratory. These included installing a remote alarm system that would notify five people instead of one. All lawsuits in this case were settled out of court, with patients signing nondisclosure agreements. It is likely the payouts to affected patients were in the millions, and they were also provided additional fertility treatments (Robbins 2023). Moreover, one family filed a wrongful death lawsuit based on the 1985 case Werling v. Sandy, where the Ohio Supreme Court declared that a “viable fetus is a person.” In 2019, the Ohio Appeals Court affirmed that embryos were not persons based on the 1973 landmark U.S. Supreme Court’s decision in Roe vs. Wade (Legal Information Institute, n.d.), which said that a fetus that developed after the embryonic state was not a person (Zhang 2018; Vaughn 2020).
All of this changed after the U.S. Supreme Court overturned Roe v. Wade in 2022 in Dobbs v. Jackson Women’s Health Organization (Supreme Court of the United States 2021; Liptak 2024), and several states have put severe restrictions on abortion rights and are working toward passing and ratifying laws that would assign personhood to embryos in their state legislatures (Pazanowski 2024; Messerly 2024; Mosley 2024). These legislative changes might also limit patients’ fertility treatment options, and ART/IVF providers might be held criminally liable in case of accidental damage or destruction of embryos, or embryo disposal at the patient’s will or in case of unclaimed embryos (Letterie 2022; Letterie and Fox 2023). Dealing with the long-term storage of unclaimed embryos had already been an ethics issue and a topic of active debate prior to the 2023 SCOTUS decision.
In a lesser-known case of a -80 ˚C freezer failure at the University of British Columbia in 2002, the fertility clinic lost the frozen sperm of ~400 patients. In January 2015, the Court of Appeal of British Columbia decided in the claimants’ favor that human sperm could be “property” and, therefore, considered as goods under the statutory provisions (Starza-Allen 2015). As a result of this court decision, patients were awarded $6.2 million in compensation, and the clinic ceased operation. In another case of a tank failure at Northwestern Memorial that led to a massive loss of sperm, one patient received a settlement of $1 million (Pfaff, Gill & Ports, Ltd. 2023).
3.3. Frozen reproductive specimen mix-ups, mishandling, loss, and damage
While individual or smaller-group cases involving embryo and sperm mix-ups are on a much smaller scale than large-scale storage, tank, and alarm failures (Table 2 and Figure 2), they are equally as devastating. There is another layer of legal, financial, reputational, emotional distress, and costs to patient families and the providers. This includes the genetic and birth parents of the child(ren) and child(ren) themselves, plus the ART/IVF providers involved in these incidents because of the systematic issues with operational, cryostorage, and record-keeping procedures at their clinics.
3.3.1. Consequences of frozen reproductive specimen mix-ups
Frozen reproductive specimen mix-ups are the most prevalent type of IVF related incident following catastrophic large-scale storage, tank, and alarm failures (Figure 2). The first widely publicized U.S. case that set a precedent for the following cases on who would get the child(ren)—genetic or birth parents—was Perry-Rogers v. Fasano (2000). In this case, a White couple, Richard and Donna Fasano, had twin sons via ART/IVF treatment, one of whom was an African American child. The newborn boy’s genetic parents, Deborah Perry-Rogers and Robert Rogers sued the Fasanos for the custody of their biological son and won. At 8 months, their son was returned to them. All the following U.S. cases of embryo mix-ups, resulting in a wrong parent carrying the child(ren) who was not biologically related to them, to term, were settled in favor of genetic parents, including Manukyan v. CHA Fertility (2019). In this particularly devastating case, an Asian couple who went to California to seek fertility treatments were expecting to have twin daughters, but instead, the mother gave birth to twin boys, who were not Asian and were not related to each other. The two other parental couples sued and successfully won the custody of their biological children, leaving the birth couple who wanted to raise the children devastated. What happened to the couple’s own two female embryos were never determined, and their case, A.P. et al v. CHA Health Systems, Inc. et al., moved from New York State to California for further litigation (2023).
In the Czech Republic, however, the law states the mother of the child(ren) is the woman who gives birth to the child(ren). Regardless of genetic maternity, the birth mother has legal rights to keep the child(ren). In case of embryo mix-ups involving international patients, who visit the Czech Republic for fertility treatments, the custody lawsuits might be complicated by the differences between the Czech law and the laws of their countries, with the Czech law taking precedent in Czech courts, regardless of the patients’ and child(ren)’ nationality. In 2017, the Reprofit clinic that provides fertility treatments to hundreds of foreign patients, most of whom are from the U.K., implanted the wrong embryos in the wombs of two mothers, both of whom were foreign nationals (Holmes 2017).
Among other severe consequences of embryo and sperm mix-ups are the loss of identity in patients and child(ren) born to a mix-up and strain in parent relationships if the child(ren) were born to a married couple or a couple in a long-term relationship, coming from the accusations of infidelity by partners, spouses, other family members, and extended community. In 2007, a couple in the Canary Islands underwent fertility treatments, and the woman gave birth to twins (Jabois 2017). However, when the nurse was performing a blood test, it did not match the partner’s blood type, and he broke up with the mother. When she sued him for child support, the DNA test proved that the twins were not biologically his, and she filed the lawsuit against the Instituto Canario de Infertilidad. The clinic’s lawyers tried to accuse her of adultery and trying to use pregnancy as a tool to capture a wealthy man as a legal argument. However, the Spanish Supreme Court reprimanded them for making archaic and defamatory allegations against the mother and awarded her and the twins $356,000. In a sperm mix-up in New Jersey, USA, in 2012, a White couple gave birth to an Asian daughter, who was also a carrier of the rare genetic disorder neither her genetic mother nor birth father had (Romo 2019). The marriage ended in divorce, and the couple sued the fertility clinic for the release of the donor list. While the clinic insisted that the husband’s sperm was used and the wife committed adultery, the court ordered the release of the list of donors to the now divorced couple because the child had the right to know the identity of her biological father, and if there were predisposition to other genetic disorders.
Several patients who gave birth to child(ren) of a different race than either or both birth parents as a result of a reproductive specimen mix-up sued the clinics for emotional distress, breach of contract, and medical malpractice. Their rationale was different: (1) while accepting of their child(ren), some were bullied by their partners/spouses, families, and local communities that were predominantly of the same race as birth parents, with the woman being the primary target of derogatory comments and accusations of adultery (Starza-Allen 2021); and (2) some were not prepared to raise a child of a different race because of personal beliefs and prejudices (CBS News, 2015). Most of these cases were dismissed by the courts as frivolous, since the child(ren) were biologically related to the mother, and having a healthy child was not the negative outcome of their fertility treatments and did not qualify as causing a severe emotional distress.
In some cases, the wrong patients who received the wrong embryos and carried those to term agree amicably on returning the child(ren) to their biological parents, such as the 2009 case of the Savage and Morell embryo mix-up in the state of Ohio (ABC News Network 2010), and the 2018 embryo mix-up case of Alexander and Daphna Cardinale and an unnamed couple in the state of California (Vigdor 2021). However, they still had to go through lengthy and expensive custody litigation. In some cases, the wrong patients who received the wrong embryos decided to abort the fetus, as reported in the U.K., Germany, and Japan (one case each), and two in the U.S. In a 2023 U.S. case, a patient who was pregnant with the wrong embryo waited until right before 6 months into her pregnancy to abort the fetus, with 6 months being the legal limit for abortions in the state of Massachusetts. The couple in this case underwent fertility treatments in New York City in the same clinic and by the same embryologist as in the Perry-Rogers v. Fasano case and are now suing the clinic and embryologist (Salcedo 2022).
Embryo mix-ups and loss carry heavy consequences for ART/IVF clinics as well. The systematic errors in record keeping and organization at Ochsner that potentially affected 125 patients led to its closure (Nosheen 2009). In 2022, when the woman gave birth to the wrong child after undergoing fertility treatments at the Assuta Medical Center in Israel, the Ministry of Health (MoH) found that the fertility clinic was overwhelmed with procedures and ordered it to stop accepting new IVF patients. The MoH also ordered the clinic to test potential parents who underwent fertility treatments at the same time as the child’s birth mother. No matches were found. At first, the MoH wanted to shut down the clinic but reconsidered their decision because the closure would cut off the valuable health service to many patients in need of fertility treatments. Instead, the Assuta Medical Center was ordered to reduce its operations in half from 10,000 to 5000 cases a year (Horowitz 2022).
3.3.2. Consequences of frozen reproductive specimen damage, loss, and destruction
In several cases concerning the same clinic, couples lost their opportunity for parenthood because of the loss, damage, and improper records kept by the clinic. In the New York Times article “Lost Embryos” (Rosman 2021), after having their only son in 1996 with the help of fertility treatments, Elaine Meyer and Barry Prizant discussed the letter they received from the clinic, telling them that they still had two embryos and asking to continue paying $500 a year for cryostorage, despite their previous belief that all their embryos were used in unsuccessful attempts to conceive. Further conversations with the fertility provider revealed that the vial with their embryos was discovered at the bottom of a tank following more than a decade of storage. The vial was cracked, which most likely damaged or destroyed them. Even if the embryos were stored properly and were viable at the time of their rediscovery, the couple had aged out of their personal family building time. In another case at the same hospital, a remarried widowed woman was unable to use the embryo she created with her late husband after receiving a similar storage invoice for the frozen embryo, she thought she did not have, thus finding out about it years after his passing (Cloutier-Bristol v. Women & Infants’ Fertility Center et al., n.d.). However, she could not use this embryo with her second husband because she did not have her late husband’s consent to use it in case of his death. These are the two examples of fertility providers not conducting thorough regular audits of their cryoinventory at a recommended frequency and failing to do routine tank maintenance over prolonged periods of time, which resulted in the loss of opportunity by their patients to conceive and fulfil their goals of parenthood. In a third case, a couple, after being asked by the facility in 2006, informed it that they wanted to use embryos for future attempts. However, in 2008, when they asked the hospital about their embryos, they were told that the hospital did not have any left. In 2008, their lawyer convinced them they had no legal case because the field was relatively new, and embryos were not considered life. They did testify at the hearing aimed to introduce the Embryo Safety and Storage Act of 2023, which would require the Department of Health to regulate and license embryo storage facilities in Rhode Island (Buteau 2019). The bill’s sponsor, Representative Bill MacNamara, came up with the proposal after learning about the Meyer-Prizant case and the overall lack of regulation of ART/IVF cryostorage facilities on the federal level (State of Rhode Island General Assembly 2024).
4. Conclusions
Regardless of the circumstances, scale, legal outcomes, and country of the known IVF incidents, we found common factors that alone or together led to the reported incidents: (1) human error, when an embryologist was distracted because of a heavy workload and multitasking, personal circumstances, or other contributing factors, and retrieved/deposited the wrong reproductive specimen from/to cryostorage; (2) paper records and hand-written labels that in some cases led to one-time mistakes and in some cases were the result of systematic issues with the clinic’s SOPs and cryomanagement processes; (3) old/defective cryostorage tanks, broken/disabled alarms, and/or insufficient safeguards in case of emergency; and (4) lack of or insufficient training of the embryology laboratory personnel and/or healthcare professionals tasked to handle frozen reproductive specimens and patient records. As indicated above, some clinics either (1) shut down and lost their license permanently or (2) were reevaluated and restructured to reduce the workload and improve the operational workflows and frozen reproductive specimen management. Despite the substantial financial, legal, and reputational costs to their patients and themselves, some clinics that avoided shutdowns and restructuring continued their operations without further changes and improvements to their workload and SOPs. Owing to the heterogeneity of legal and regulatory landscapes re: the ART/IVF industry worldwide, as well as cultural/personal restrictions that prevent patients from telling their stories and/or non-disclosure agreements after out-of-court settlements, we can only make educated estimates about the true scope of the issue and its financial cost to ART/IVF providers, which might range from thousands to millions of USD. Digitization of records, automated handling of specimens and AI on the one hand, and updating SOPs and improving training, work conditions, and workplace culture at ART/IVF clinics on another should reduce the risks of potential errors, lessen the burden on embryologists, and allow for more precise and patient- and specimen-friendly cryomanagement of frozen reproductive specimens.
Funding
This study was supported by TMRW Life Sciences, without any external funding.
Conflicts of Interests
Michael G. Collins is an employee and a stockholder of TMRW Life Sciences. Anar Murphy has no conflicts of interest to declare.
Acknowledgements
We would like to thank Nalini Saxena of Elicit Consulting and her team for assistance setting up the initial database and identifying the first 45 cases used in this study. We would also like to thank Gustavo Hernandez, a Freshman at the Fu Foundation School of Engineering and Applied Science at Columbia University, and Julia Stork, a Senior at the Weinberg College of Arts and Sciences at Northwestern University, for providing editorial support.